Not all strep infections are alike and it may have nothing to do with you
One person infected with strep bacteria might get a painful sore throat; another might face a life-threatening blood infection. Now, scientists are trying to pin down why.
Variation between individuals’ immune systems may not be entirely to blame. Instead, extra genes picked up by some pathogens can cause different strains to have wildly different effects on the immune system, even in the same person, researchers report January 11 in PLOS Pathogens.
The idea that different strains of bacteria can behave differently in the body isn’t new. Take E. coli: Some strains of the bacteria that can cause foodborne illness make people far sicker than other strains. But bacteria have exceptionally large amounts of genetic variation, even between members of the same species. Scientists are still trying to figure out how that genetic diversity affects the way microbes interact with the immune system.
Any species of bacteria has a core set of genes that all its members share. Then there’s a whole pot of genes that different strains of the species pick and choose to create what’s known as an accessory genome. These genes are custom add-ons that specific strains have acquired over time, from their environment or from other microbes — something like an expansion pack for a card game. Sometimes, that extra genetic material gives bacteria new traits.
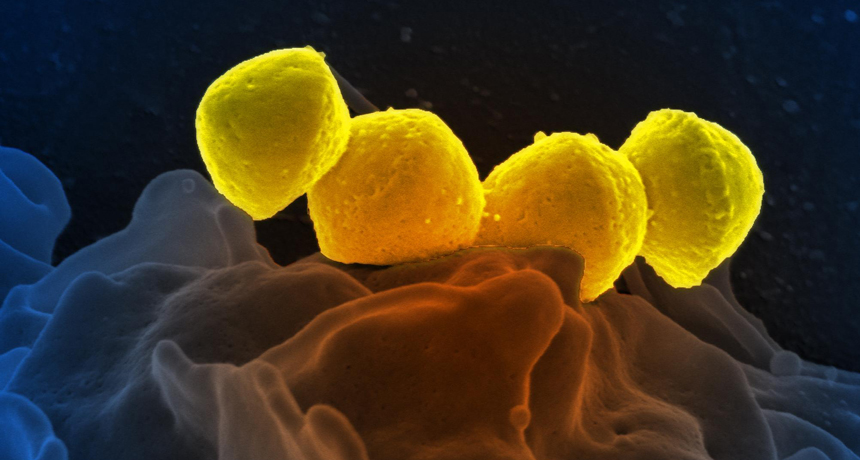
Uri Sela and his colleagues at the Rockefeller University in New York City tested the way these extra genes influenced the way two common species of bacteria, Staphylococcus aureus and Streptococcus pyogenes, interacted with the immune system. Staphylococcus bacteria can cause everything from rashes to food poisoning to blood infections. Streptococcus bacteria can cause strep throat, as well as a host of more serious illnesses (SN: 10/4/14, p. 22).
Different strains of the same species provoked wildly different immune responses in blood samples collected from the same patient, the researchers first showed. But the strain-specific responses were consistent across patients. Some strains triggered lots of T cells to be made in every sample, for example; others increased B cell activity. (T cells and B cells are the two main weapons of the adaptive immune response, which enables the body to build long-lasting immunity against a particular pathogen.) In tests of strains missing some of their extra genes, though, the T cells didn’t respond as strongly as they did to a matching strain that contained the extra genes. This finding suggests that the variation in immune response across strains was coming, at least in part, from differences in these supplementary genes.
“Currently when a patient comes to the hospital with an infection, we don’t define the strain of the species” for common infections like strep and staph, says Sela, an immunologist. In the future, he says, information about the strain could help doctors predict how a patient’s illness will unfold and decide on the best treatment.
The new study “adds fuel to an active debate” about the role of accessory genes, says Alan McNally, a microbiologist at the University of Birmingham in England — whether or not the collections of genetic add-ons that bacteria maintain are shaped by natural selection, the process that fuels evolution. This research suggests that for some kinds of bacteria, genetic customization might aid survival of certain strains by enabling them to provoke a tailored immune response.
But more research needs to be done to link the strain-to-strain variation in immune response to the accessory genome, he says, as this study looked at only a few extra genes, not the entire accessory genome.